What causes perianal fistula? This question is common among people experiencing discomfort or unusual symptoms near the anus. A perianal fistula, also known as an anal fistula, is an abnormal tunnel between the anal canal and the skin near the anus. Understanding the causes of this condition is essential to prevent complications and get the right treatment.
In this blog, we will explore the key factors behind perianal fistula formation. We will explain how infections, chronic diseases, injuries, and other causes contribute to this painful condition. Along the way, you will learn about the most common causes, risk factors, and how your lifestyle or health conditions may increase your chances of developing a fistula. Let’s get started.
What Causes Perianal Fistula? The Basics
The main cause of a perianal fistula is an infection in the small anal glands. These glands are located inside the anus and help lubricate the anal canal. When bacteria enter these glands, they can cause an infection, leading to the formation of an abscess. An abscess is a painful collection of pus caused by the body’s attempt to fight the infection.
If this abscess does not heal properly, it can form a tunnel or fistula between the infected gland and the skin around the anus. This tunnel allows pus or other fluids to drain, often causing pain, swelling, and discharge. This is the classic cause of most perianal fistulas.
Other causes can include trauma, chronic inflammatory diseases, or previous surgery in the anal area. However, infection of the anal glands remains the leading cause. It is important to understand how and why this infection develops, so you can recognize the risk factors and seek timely care.
Anal Fistula Causes: Infection and Abscess Formation
Infections are the root cause of most perianal fistulas. The anal glands can become blocked or injured, allowing bacteria to multiply and cause abscess formation. This infection can be caused by several factors:
1. Blockage of Anal Glands
The small anal glands can become blocked by stool, dirt, or hair. When the glands cannot drain properly, bacteria get trapped inside. This blockage increases the risk of infection and abscess formation.
2. Poor Hygiene
Not cleaning the anal area properly after bowel movements can increase bacteria buildup. As a result, this environment makes it easier for infections to develop in the anal glands. Additionally, poor hygiene can contribute to irritation and inflammation, further raising the risk of infection.
3. Trauma or Injury
Any injury to the anal or rectal area can introduce bacteria into the glands. For example, surgical wounds, childbirth tears, or accidents that damage the skin near the anus may lead to infection. Therefore, such injuries increase the risk of developing a fistula.
4. Constipation or Straining
Hard stools and excessive straining can cause tiny tears or pressure on the anal glands. These small injuries make it easier for bacteria to invade the tissue and start an infection.
Once the infection starts, the body tries to fight it by sending white blood cells to the area. This causes swelling and pus formation, resulting in an abscess. If the abscess is not treated properly or bursts inside the tissue, it can lead to fistula formation.
Perianal Fistula Risk Factors: Who Is Most Likely to Develop It?
Certain conditions and habits increase the risk of developing a perianal fistula. Understanding these perianal fistula risk factors can help you take preventive steps.
1. Crohn’s Disease
Crohn’s disease is an inflammatory bowel disease that causes chronic inflammation of the digestive tract. People with Crohn’s often develop fistulas due to persistent inflammation and damage to the intestinal wall. In fact, Crohn’s disease is one of the most common underlying causes of complex or multiple perianal fistulas.
2. Previous Anal Abscess
If you have had an anal abscess in the past, you are more likely to develop a fistula. This is because the abscess may not have healed fully or the infection spread into the surrounding tissue.
3. Gender and Age
Perianal fistulas are more common in men than women. They also tend to affect adults between 20 and 40 years of age.
4. Smoking
Smoking weakens the immune system and reduces blood flow to the tissues. Consequently, this slows healing and increases the chance of infection and fistula formation.
5. Obesity
Moreover, excess weight can increase pressure on the pelvic and anal area. Consequently, this added pressure can cause small injuries and reduce healing capacity.
6. Chronic Diarrhea or Constipation
Frequent diarrhea or constipation can irritate the anal region. Furthermore, both conditions raise the risk of infections in the anal glands.
Other Causes of Fistula: Trauma and Surgery
In addition to infection and inflammation, trauma and surgery can cause perianal fistula. For example:
- Surgical procedures in the anal or rectal area sometimes damage glands or tissues. This damage can cause abnormal tunnels to form as the body tries to heal.
- Childbirth with tears or episiotomy cuts can also increase the risk.
- Injuries such as cuts, burns, or blunt trauma near the anus may introduce bacteria and start an infection leading to fistula formation.
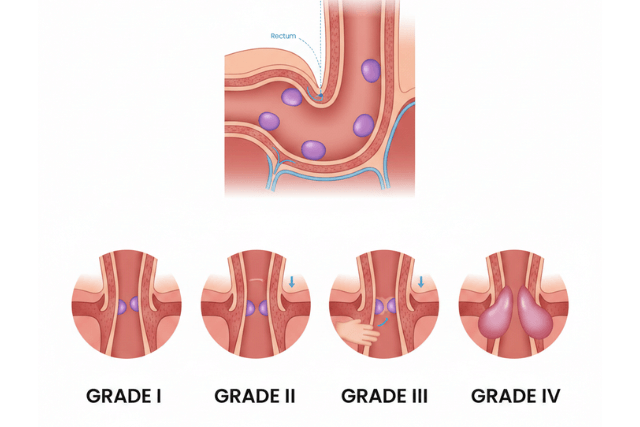
Understanding the Anatomy: How Does a Fistula Form?
To begin with, understanding what causes perianal fistula requires knowing the anatomy of the anal area. Specifically, the anal canal contains several tiny glands that open into it. These glands produce mucus, which helps stool pass easily.
When one or more of these glands become infected, the infection can create a path through the tissues, thus forming a tunnel or fistula. Typically, this fistula connects the infected gland inside the anal canal to the skin near the anus. In many cases, the opening on the skin is visible as a small bump or sore.
This fistula can drain pus or fluids, which leads to ongoing irritation and discomfort. If left untreated, the fistula may persist for months or even years. Therefore, timely diagnosis and treatment are essential to prevent long-term complications.
The Role of Inflammatory Diseases in Fistula Formation
Chronic inflammatory diseases like Crohn’s and ulcerative colitis cause ongoing inflammation in the digestive tract. This inflammation damages the lining and tissues. Over time, this damage can lead to abscesses and fistulas.
People with Crohn’s disease are especially vulnerable because the inflammation can extend beyond the intestine to the surrounding tissues. Perianal fistulas in these patients can be more complex and harder to treat.
Proper management of inflammatory bowel disease can reduce the risk of fistula formation. This includes medication, diet changes, and regular check-ups with a healthcare provider.
Infection Control: Preventing What Causes Perianal Fistula
Preventing infection is key to reducing the risk of perianal fistula. You can take several simple steps:
- Practice good anal hygiene by cleaning the area gently after bowel movements. Use mild soap and water, and avoid harsh chemicals.
- Manage bowel habits by avoiding constipation and diarrhea. Eat a fiber-rich diet and stay hydrated.
- Treat any anal abscesses or infections promptly with medical help.
- Avoid prolonged sitting or pressure on the anal area when possible.
- If you have Crohn’s disease or other inflammatory conditions, follow your treatment plan closely.
When to See a Doctor About Perianal Fistula
If you notice symptoms such as persistent pain, swelling, discharge of pus or blood, or skin irritation near your anus, see a healthcare professional. Early diagnosis and treatment can prevent complications.
Doctors use physical exams, imaging, and sometimes surgery to confirm a fistula. Treatment depends on the cause, fistula complexity, and your overall health.
Conclusion:What Causes Perianal Fistula?
What causes perianal fistula? Most often, it begins with infection of the anal glands leading to abscess formation and a tunnel to the skin. Other key factors include chronic inflammatory diseases, trauma, and lifestyle risks such as smoking and poor hygiene.
Knowing these causes and risk factors can help you take steps to prevent this painful condition. If you experience symptoms, seek prompt medical attention to avoid complications. Proper care and treatment can help you heal fully and return to a healthy life.