Hemorrhoids are a common condition that affects many individuals worldwide, often causing discomfort and pain. While some people may experience minor symptoms, others can suffer from more severe issues, such as prolapsed hemorrhoids. Understanding prolapsed hemorrhoids is essential for those dealing with the condition, as it can help manage symptoms and seek appropriate treatment.
This blog will provide a comprehensive guide on prolapsed hemorrhoids, thus covering everything from symptoms to treatment options.
What Are Prolapsed Hemorrhoids?
Understanding prolapsed hemorrhoids begins with understanding hemorrhoids themselves. Hemorrhoids are swollen veins located in the rectum or anus. They occur when the blood vessels around the anus or lower rectum become swollen due to pressure. Prolapsed hemorrhoids are a more severe form of this condition, where the hemorrhoid bulges out of the anus.
Prolapsed hemorrhoids occur when the tissue supporting the hemorrhoid weakens or stretches, causing the hemorrhoid to slip out of its normal position. This condition can be quite uncomfortable and may lead to a variety of symptoms. It’s important to note that prolapsed hemorrhoids can be classified into four grades, depending on their severity.
Symptoms of Prolapsed Hemorrhoids
understanding the symptoms of prolapsed hemorrhoids is crucial for early intervention. The signs can range from mild to severe, depending on the grade of the prolapsed hemorrhoid. Below are the most common symptoms associated with this condition:
1. Rectal Bleeding
One of the most noticeable symptoms of prolapsed hemorrhoids is rectal bleeding. This often occurs when the swollen veins rupture due to the pressure exerted during bowel movements. Blood may appear on toilet paper or in the toilet bowl, typically bright red in color.
2. Pain and Discomfort
Prolapsed hemorrhoids can cause significant discomfort, particularly during or after bowel movements. The pain may be sharp, throbbing, or a dull ache in the affected area. This discomfort is often a result of inflammation or irritation of the prolapsed hemorrhoid.
3. Itching and Irritation
Itching around the anus is another common symptom of prolapsed hemorrhoids. This itching can be caused by mucus discharge or irritation of the skin around the anus. The constant irritation can worsen if not managed properly.
4. Swelling and Lumps Around the Anus
In more severe cases, prolapsed hemorrhoids may cause swelling or the appearance of lumps around the anus. These lumps can be felt when you gently press around the anus. Prolapsed hemorrhoids may also appear as a visible bulge outside the anus.
5. Difficulty Cleaning After Bowel Movements
People with prolapsed hemorrhoids often find it challenging to clean the area around the anus after a bowel movement. This can result in further irritation and discomfort, making it important to use gentle cleaning methods and proper hygiene.
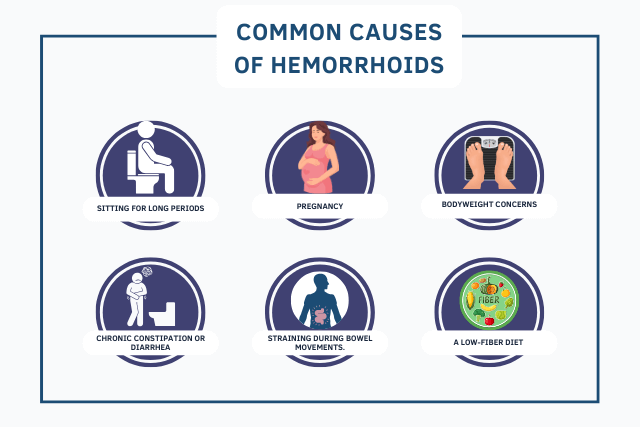
Causes of Prolapsed Hemorrhoids
Several factors can contribute to the development of prolapsed hemorrhoids. These include lifestyle choices, genetic factors, and underlying medical conditions. Here are the most common causes:
1. Chronic Constipation
Chronic constipation is a major risk factor for developing prolapsed hemorrhoids. Straining during bowel movements puts pressure on the veins in the rectal area, leading to swelling and the potential for prolapse.
2. Pregnancy
Pregnancy poses a higher risk of developing prolapsed hemorrhoids due to increased pressure on the pelvic region and hormonal changes. The added weight and pressure can weaken the tissues around the anus, thus causing hemorrhoids to prolapse.
3. Obesity
Obesity can increase the risk of hemorrhoids, including prolapsed hemorrhoids. Extra weight puts pressure on the lower abdomen and rectum, which can lead to swollen veins and the potential for prolapse.
4. Aging
As people age, the tissues around the anus and rectum can weaken and stretch. This can make older adults more susceptible to prolapsed hemorrhoids, especially if they have a history of constipation or other contributing factors.
5. Sitting for Long Periods
Sitting for extended periods of time, particularly on the toilet, can increase the pressure on the veins in the rectum. This can contribute to the development of prolapsed hemorrhoids over time.
Diagnosis of Prolapsed Hemorrhoids
Diagnosing prolapsed hemorrhoids typically begins with a physical examination by a healthcare provider. During the exam, the doctor will check for visible signs of prolapsed hemorrhoids and assess their severity. In some cases, additional tests, such as a rectal exam or anoscopy, may be needed to confirm the diagnosis.
Treatment Options for Prolapsed Hemorrhoids
Treating prolapsed hemorrhoids depends on the severity of the condition. In many cases, lifestyle changes and home remedies can alleviate symptoms. However, more severe cases may require medical intervention or surgery. Here are the most common treatment options:
1. Dietary Changes
Increasing fiber intake can help prevent constipation and reduce the strain on the rectum during bowel movements. A diet high in fruits, vegetables, and whole grains can soften stools and promote regular bowel movements, reducing the risk of prolapsed hemorrhoids.
2. Topical Treatments
Topical creams and ointments are often used to relieve the pain and discomfort associated with prolapsed hemorrhoids. In addition, these treatments can help reduce inflammation, soothe itching, and promote healing.
3. Sitz Baths to relieve pain associated with prolapsed hemorrhoids
A sitz bath is a warm, shallow bath that soothes the affected area. Soaking in a sitz bath for 10–15 minutes several times a day can help reduce inflammation and, therefore relieve pain associated with prolapsed hemorrhoids.
4. Over-the-Counter Medications
Over-the-counter medications, such as pain relievers or stool softeners, can help manage the symptoms of prolapsed hemorrhoids. Pain relievers like acetaminophen or ibuprofen can help reduce discomfort, while stool softeners make bowel movements easier and less painful.
5. Rubber Band Ligation
For more severe cases of prolapsed hemorrhoids, a doctor may recommend rubber band ligation. This procedure involves placing a small rubber band around the base of the hemorrhoid, thus cutting off its blood supply. This causes the hemorrhoid to shrink and fall off within a few days.
6. Sclerotherapy
Sclerotherapy is a non-surgical treatment for prolapsed hemorrhoids that involves injecting a chemical solution into the hemorrhoid. This solution causes the hemorrhoid to shrink and eventually be reabsorbed by the body.
7. Hemorrhoidectomy
In cases where prolapsed hemorrhoids do not respond to other treatments, a hemorrhoidectomy may be necessary. Specifically, this surgical procedure involves removing the hemorrhoids to provide long-term relief. Moreover, it is typically reserved for severe or persistent cases.
8. Laser Hemorrhoidoplasty (LHP®): Laser Treatment For Hemorrhoids
One of the newer and highly effective treatment options for prolapsed hemorrhoids is Laser Hemorrhoidoplasty (LHP®). This procedure uses laser technology to shrink and treat hemorrhoids without the need for traditional surgery. LHP® is minimally invasive, meaning it requires no incisions or stitches. The laser energy targets the blood vessels in the hemorrhoids, causing them to coagulate and shrink. This treatment is typically faster than traditional methods, with a quicker recovery time. Patients often experience less pain and bleeding after the procedure compared to more invasive options.
Laser Hemorrhoidoplasty (LHP®) is an excellent option for those looking for a modern, less invasive way to treat prolapsed hemorrhoids. Additionally, the treatment offers a high success rate and is suitable for individuals who want to avoid the longer recovery times associated with surgery.

Preventing Prolapsed Hemorrhoids
While prolapsed hemorrhoids can be difficult to prevent entirely, there are several steps you can take to reduce your risk:
1. Eat a High-Fiber Diet to prevent prolapsed hemorrhoids.
Consuming a fiber-rich diet can help prevent constipation and reduce the risk of developing prolapsed hemorrhoids. In addition, fiber helps soften stools and promotes regular bowel movements, making it an essential part of digestive health.
2. Stay Hydrated
Drinking plenty of water throughout the day can help keep stools soft and prevent constipation, thus leading to prolapsed hemorrhoids.
3. Exercise Regularly to prevent prolapsed hemorrhoids.
Regular physical activity can help improve circulation and reduce the pressure on the veins in the rectum. Exercise also helps prevent constipation, which is a major risk factor for prolapsed hemorrhoids.
4. Avoid Straining During Bowel Movements
Straining during bowel movements puts unnecessary pressure on the veins in the rectal area. Avoiding this strain can help reduce the risk of developing prolapsed hemorrhoids.
Conclusion: Understanding Prolapsed Hemorrhoids
Understanding prolapsed hemorrhoids is crucial for anyone experiencing symptoms related to this condition. By recognizing the signs early and seeking appropriate treatment, you can alleviate discomfort and prevent the condition from worsening. Whether through dietary changes, topical treatments, or medical procedures, there are numerous ways to manage and treat prolapsed hemorrhoids effectively.
If you suspect you have prolapsed hemorrhoids, it’s essential to consult with a healthcare professional to determine the best course of action for your individual needs.