Pilonidal Disease causes pain and discomfort but understanding it well can help you prevent and manage it effectively. In this detailed guide, we will cover the causes, symptoms, prevention methods, and treatment options for Pilonidal Disease:. You’ll learn everything you need to know to take control of this condition.
What is Pilonidal Disease?
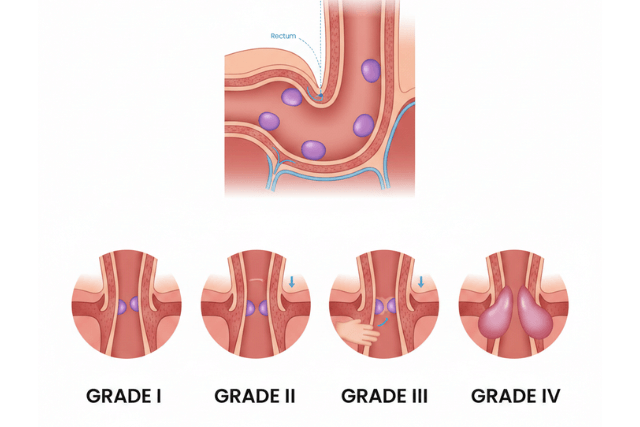
First, let’s define Pilonidal Disease: clearly. Pilonidal Disease is a chronic skin condition that occurs near the tailbone, usually at the top of the cleft between the buttocks. It happens when hair and debris get trapped under the skin, causing painful cysts or abscesses. The word “pilonidal” means “nest of hair,” which highlights the role of hair in this condition.
Pilonidal Disease commonly affects young adults, especially men. It can range from mild irritation to severe infection requiring surgery. Understanding the Pilonidal Disease causes is key to managing and preventing it.
Pilonidal Disease Causes
One of the main reasons Pilonidal Disease develops is hair penetrating the skin in the buttocks crease; consequently, this penetration triggers an inflammatory response, forming cysts or sinus tracts.
Several factors contribute to this condition:
Hair Growth and Ingrown Hair
Loose hair fragments tend to collect in the cleft. When these hairs grow inward or get pushed into the skin, they cause irritation and inflammation.
Prolonged Sitting
Sitting for long hours increases pressure on the tailbone area. This pressure forces hair and debris into the skin, raising the risk of pilonidal cysts.
Friction and Skin Trauma
Repeated rubbing or minor injuries in the crease can break the skin barrier. This allows hair to penetrate and start the disease process.
Poor Hygiene
Lack of regular cleaning allows sweat, dead skin cells, and loose hairs to build up. This buildup can worsen irritation and infection risk.
Obesity
Extra body weight causes deeper skin folds and increased sweating. These conditions create a moist environment favorable to cyst formation.
Family History
Genetics may play a role. People with relatives who had pilonidal disease are more likely to develop it.
Pilonidal Disease Symptoms
Recognizing Pilonidal disease symptoms early helps you seek treatment promptly, as symptoms may range from mild discomfort to severe infection.
Pain and Tenderness
Pain near the tailbone or buttocks crease usually signals the start. The pain worsens when sitting, standing, or walking for long periods.
Swelling and Redness
The affected area often becomes swollen, tender, and red, which are signs of inflammation or infection.
Drainage of Pus or Blood
An infected cyst may drain pus or blood through a small opening near the crease.
Fever and Malaise
If infection spreads, fever, chills, and a general feeling of illness can occur.
Visible Lump or Cyst
You may notice a small bump or cyst under the skin near the tailbone.
Pilonidal Disease Prevention
Preventing Pilonidal Disease involves reducing risk factors and, therefore, keeping the area clean. Here are effective prevention strategies.
Maintain Good Hygiene
Regularly clean the buttocks crease daily with mild soap and water to effectively remove dirt and loose hairs.
Keep the Area Hair-Free
Regular hair removal, such as shaving or laser hair removal, prevents hair buildup. Be careful when shaving to avoid skin irritation.
Avoid Prolonged Sitting
Take breaks to stand and move if you sit for long periods at work or school.
Wear Loose Clothing
Tight clothes cause friction and trap sweat; however, loose, breathable fabrics help keep the area dry and reduce irritation.
Manage Body Weight
Losing excess weight reduces skin folds and sweating, thus lowering the risk.
Control Sweating
Use powders or antiperspirants to keep the area dry, especially if you sweat heavily.
Pilonidal Disease Treatment Options
Treatment depends on how severe your condition is. Some cases improve with home care, while others require medical procedures.
Conservative Treatment For Pilonidal Disease
For mild symptoms, doctors recommend:
- Warm compresses to reduce pain and swelling.
- Keeping the area clean and dry.
- Regular hair removal to prevent recurrence.
- Over-the-counter pain relievers for discomfort.
Incision and Drainage
If the cyst becomes infected or forms an abscess, a doctor will drain the pus by making a small cut. This relieves pain and clears infection but does not remove the cyst completely.
Surgical Removal For recurrent or severe pilonidal disease
For recurrent or severe pilonidal disease, surgery is often necessary; therefore, the surgeon removes the cyst and infected tissue. Surgical methods include:
- Excision with open healing: The wound is left open to heal from inside out, reducing recurrence risk but requiring longer healing time.
- Primary closure: The wound is closed with stitches immediately after removal. This allows faster healing but may have a higher chance of recurrence.
- Flap surgery: Tissue is rearranged to cover the wound, reducing tension and lowering recurrence.
SiLaC® (Sinus Laser Closure) Treatment
An innovative, minimally invasive option is SiLaC®, which actually uses laser energy to close the sinus tract without removing large amounts of tissue.
- The surgeon inserts a laser fiber into the sinus tract through a small incision.
- The laser destroys the infected tissue and seals the tract.
- SiLaC® reduces pain, shortens recovery, and lowers recurrence risk.
- It is suitable for selected patients, especially those with smaller or less complex cysts.
Although promising, long-term data is still being studied. SiLaC® complements traditional surgery but does not replace it in all cases.
Laser Hair Removal
Laser hair removal reduces hair growth in the affected area; furthermore, this procedure can prevent new cysts from forming after treatment or surgery.
Living with Pilonidal Disease: What to Expect
If you have Pilonidal Disease:, keep these points in mind:
- Early treatment improves outcomes. Don’t delay seeing a doctor.
- Wound care is crucial after surgery. Follow your doctor’s instructions carefully.
- Recurrence can happen, but good hygiene and hair removal lower risks.
- Discuss pain management and recovery plans with your healthcare provider.
When to See a Doctor
Seek professional help if you notice:
- Increasing pain or swelling near the tailbone.
- Fever, chills, or signs of spreading infection.
- Persistent or worsening drainage.
- Recurrence of symptoms after prior treatment.
- Prompt care reduces complications and speeds healing.
Frequently Asked Questions About Pilonidal Disease
Q: Can pilonidal disease heal without surgery?
A: Mild cases might improve with hygiene and hair removal, but infected cysts usually need medical treatment.
Q: Is pilonidal disease contagious?
A: No, it is not contagious. It results from hair and skin irritation.
Q: How long does surgery recovery take?
A: Recovery can take 4-6 weeks or, however, may take longer in some cases depending on the procedure and wound care.
Q: Does laser treatment cure pilonidal disease?
A: Laser treatments like SiLaC® reduce symptoms and recurrence but may not suit all cases.
Conclusion: Understanding Pilonidal Disease
Understanding Pilonidal Disease causes and symptoms is, therefore, essential for prevention and timely treatment.
Maintaining hygiene, removing hair, and reducing pressure on the tailbone area help prevent this painful condition. When treatment is needed, options range from home care to innovative procedures like SiLaC® laser closure and traditional surgery.
Remember, early diagnosis and proper care improve outcomes significantly. If you suspect pilonidal disease, don’t hesitate to seek medical advice. Following this guide will empower you to manage pilonidal disease confidently and live comfortably.