Experiencing Recurring Abscesses is an incredibly painful and deeply frustrating ordeal for many patients today. A perianal abscess represents an acute, pus-filled infection that forms near the anus or rectum quickly. While initial drainage provides welcome and immediate infection relief, the problem often returns stubbornly. This cycle of healing and relapse indicates a deeper, hidden issue within the anal anatomy constantly. We must understand that most Recurring Abscesses are not isolated infections at all. They are actually the acute phase of a more serious, chronic anorectal disease known as an anal fistula. We specialize in diagnosing this underlying issue for successful, lasting recovery.
The Hidden Cause: From Acute Infection to Chronic Anorectal Disease
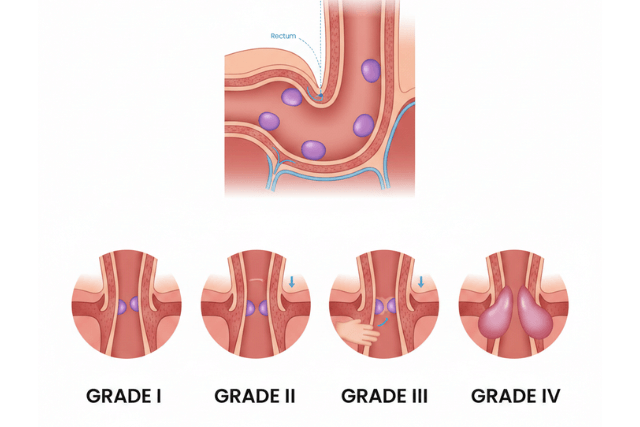
Recurring Abscesses almost always originate from one single source: a blocked anal gland inside the anal canal. We have numerous small glands in the anal canal that help with lubrication normally. If a gland opening becomes blocked by bacteria or fecal matter, the infection quickly forms pus immediately. This pus collection creates the intensely painful abscess you feel externally. When the abscess is drained, either surgically or spontaneously, the pus escapes effectively. However, the initial infection channel, or tunnel, usually remains open internally. This persistent tunnel connecting the anal gland to the skin surface is known as an anal fistula.
- The abscess represents the acute infection phase of the problem now.
- The anal fistula represents the chronic anorectal disease problem now.
- The fistula tunnel allows bacteria to continuously re-enter the internal gland effectively.
- Consequently, the tunnel becomes re-infected, leading to the recurrent pus accumulation immediately.
- We know that between 30% and 50% of patients with an abscess will eventually develop a persistent fistula constantly.
Signs Indicating Recurrent Abscesses Mean a Fistula
We recognize that persistent drainage and reoccurring swelling signal an underlying problem strongly. If a patient experiences a second abscess in the same location, a fistula is highly likely to be present. We encourage patients not to wait for the next flare-up to seek specialist treatment now. Early diagnosis of this anorectal disease is entirely crucial for preserving continence successfully.
Key Signs of an Underlying Fistula:
- Continuous Drainage: A small, persistent discharge of pus or serous fluid occurs at the old abscess site constantly.
- Healing Then Swelling: The external wound closes temporarily, but pain and swelling quickly return repeatedly.
- Visible External Opening: A tiny hole is visible near the anus that may ooze discharge consistently.
- Pain on Sitting: Severe, deep anal pain persists or returns, especially when the external opening closes temporarily.
- Recurrence Frequency: Experiencing more than one instance of an abscess confirms a chronic problem urgently.
Advanced Diagnosis: Mapping the Fistula Tract Precisely
Treating recurring abscesses effectively requires us to first precisely map the entire underlying fistula tract. However, simple physical examination is often not sufficient for identifying the complex tunnel branches. Therefore, we utilize advanced imaging modalities for complete visualization. Ultimately, our diagnostic goal is minimizing surgical complications and thus ensuring a definitive cure.
- Magnetic Resonance Imaging (MRI): We consider MRI the preferred imaging test for complex or high fistulas. Specifically, MRI provides extremely detailed images of the tract’s course and its relationship to the surrounding sphincter muscles.
- Endoanal Ultrasound (EUS): This specialized ultrasound uses sound waves to create clear images of the anal sphincter muscles. In addition, EUS helps us delineate the anatomy and identify any associated abscess cavities.
- Examination Under Anesthesia (EUA): Our surgeons examine the area thoroughly under anesthesia in the operating room. Consequently, this crucial step helps us reliably locate the internal opening of the chronic tract.
Overall, accurate mapping confirms the complexity and guides our choice of procedure immediately.
Factors Increasing the Risk of Recurrent Abscesses
We know that certain underlying conditions significantly raise the risk of developing Recurring Abscesses constantly. Addressing these systemic health issues is a fundamental part of our treatment strategy overall. Successful infection relief relies on managing these predisposing factors effectively.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease cause chronic inflammation in the intestinal tract. This inflammation often leads directly to complex and severe perianal abscesses and fistulas consistently.
- Diabetes Mellitus: Poorly controlled blood sugar impairs the body’s natural wound healing process severely. Patients with diabetes face a higher risk of non-healing or recurrent abscesses frequently.
- Immunosuppression: Medications used for autoimmune conditions or diseases like HIV weaken the immune system greatly. A weakened immune defense struggles to achieve complete infection relief successfully.
- Obesity: Patients with a higher body mass index face increased risk of both recurrence and subsequent fistula formation often. We must integrate weight management into their long-term care plan constantly.
Comprehensive Treatment for Lasting Recovery
The treatment of choice for Recurring Abscesses involves surgically eradicating the hidden fistula tract now. The goal is achieving complete infection relief while also carefully preserving the anal sphincter muscle complex entirely. Preserving the sphincter muscle is absolutely necessary for maintaining normal bowel control now. We select a procedure based entirely on the tract’s complexity and its relationship to the sphincter muscle.
Advanced Surgical Options We Offer:
- Fistulotomy: We open the entire length of a simple, low-lying fistula tract successfully. This allows the wound to heal completely from the inside out now.
- Seton Placement: We insert a special surgical drain (seton) into more complex, high-risk tracts often. The seton helps drain chronic infection and fibrosis before the definitive operation later.
- LIFT Procedure: This modern technique avoids cutting the sphincter muscle completely. We access and close the fistula tract in the tissue space between the sphincter muscles efficiently.
- Flap Procedures: We use healthy tissue flaps from the rectum to cover the internal opening for high, complex fistulas now. This method drastically reduces the risk of fecal incontinence significantly.
Why Choose IBI Clinic for Anorectal Disease Management
Choosing the right specialist is the most critical decision for successful, lasting recovery from a fistula. At IBI Clinic, we provide the comprehensive and highly specialized care necessary for complex anorectal disease now. Our board-certified surgeons and specialists possess extensive experience in treating recurring and non-healing fistulas effectively.
- Diagnostic Excellence: We use advanced MRI and EUS imaging to accurately map the entire fistula tract before any surgery now. This precise mapping is completely vital for minimizing the risk of recurrence and incontinence overall.
- Focus on Preservation: We prioritize sphincter muscle preservation above all else during every procedure we perform. Our advanced techniques, like the LIFT procedure, protect your continence long-term.
- Integrated Care: We collaborate with gastroenterologists to identify and manage underlying issues like IBD or diabetes consistently. This comprehensive approach maximizes infection relief and ensures your lasting recovery effectively.
- Cutting-Edge Technology: We offer the latest minimally invasive techniques to reduce pain and significantly speed up your healing process constantly. We commit to supporting your return to a comfortable, normal life quickly.
We are ready to end the cycle of painful Recurring Abscesses for you today. Trust the IBI Clinic team for expert, compassionate care and a successful, lasting recovery now.